Patellofemoral pain syndrome (PFPS) is a common condition affecting people across various age groups and activity levels.
Patellofemoral pain, often experienced by athletes and individuals with active lifestyles, can be challenging to manage and treat. This comprehensive guide delves into the complexity of patellofemoral pain, discussing its causes, associated injuries, and the importance of tailoring rehab programs to each patient’s specific needs.
We will also explore the significance of understanding the kinetic chain and addressing various factors such as sleep, strength training, and footwear in the treatment process.
Understanding Patellofemoral Pain Syndrome
PFPS is an umbrella term that refers to pain originating from the patellofemoral joint or the surrounding soft tissues, typically located in the anterior knee region. This condition can affect individuals differently, from an obese 13-year-old with no sports participation to a 45-year-old ultra-marathon runner.
The causes and risk factors for PFPS may vary significantly among patients, making it crucial to adopt a tailored approach when assessing and treating this condition.
Risk Factors and Assessment
To identify the specific risk factors affecting a patient with PFPS, healthcare professionals should carefully listen to the patient’s subjective experiences and use that information to guide the objective assessment.
Common risk factors for PFPS include muscle strength, muscle length, and movement control. By examining these factors, healthcare professionals can develop a bespoke assessment and treatment plan that targets the patient’s unique needs.
The Kinetic Chain and Its Impact on Patellofemoral Pain

The kinetic chain is a series of interconnected segments in the body that work together to perform movement. When it comes to patellofemoral pain, the chain starts at the foot, where excessive pronation can cause issues.
It continues through the knee, assessing rotation and movement, up to the hip, where excessive or uncontrolled femoral internal rotation and contralateral pelvic drop may occur.
Finally, it reaches the trunk, where instability may manifest in various planes. By understanding the key components of the kinetic chain and their impact on the patellofemoral joint, medical professionals can better diagnose and treat this condition.
Strength Training: Not a One-Size-Fits-All Solution
While improving strength is often a key component of patellofemoral pain treatment, it is not always the primary solution.
Some patients may already possess adequate strength but need adjustments in footwear, orthotics, or specific muscle targeting to address their pain.
It is vital for medical professionals to carefully select exercises that will target specific muscle groups without aggravating the patient’s condition.
1. Targeted exercises for patellofemoral pain
One of the keys to addressing patellofemoral pain is identifying specific exercises that target the affected area. This includes exercises that focus on hip and pelvis control, as well as femoral rotation control.
These exercises should be tailored to the individual’s needs, addressing any weaknesses or imbalances that may be contributing to the pain.
2. Adjuncts for patellofemoral pain management
In addition to targeted exercises, several adjuncts can be used to help manage patellofemoral pain. These include:
- Taping techniques: Taping can help reduce pain, improve movement, and facilitate better engagement with exercises.
- Proprioceptive work: Enhancing fine motor control can improve stability and reduce the risk of injury.
- Stretching and foam rolling: These techniques can help reduce muscle tightness and improve muscle fiber alignment, particularly in individuals with hypertrophied muscles.
- Ice massage and orthotics: Ice massage can help manage inflammation and pain, while orthotics can address foot and ankle issues that contribute to patellofemoral pain.
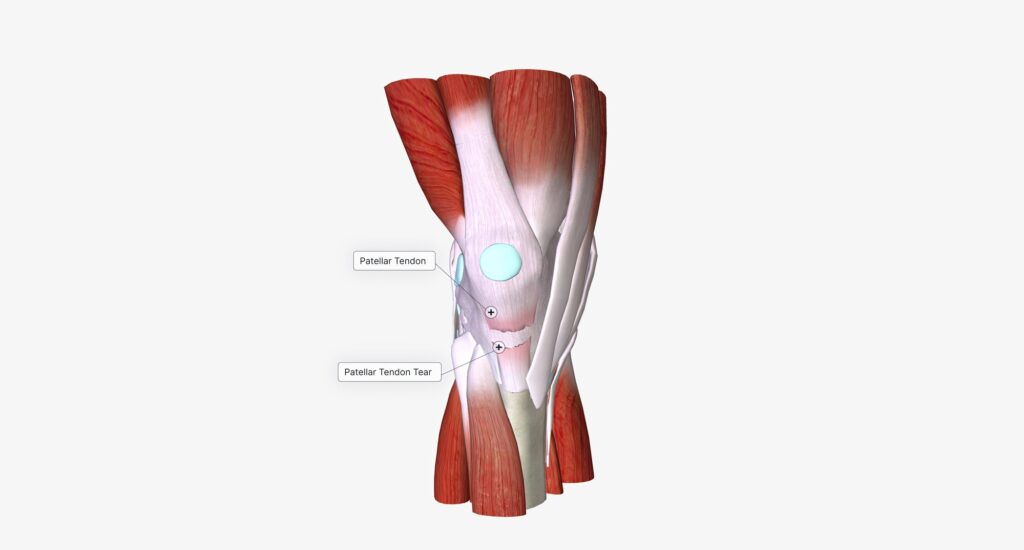
3. Identifying patellar instability
Identifying patellar instability is crucial in managing patellofemoral pain effectively. There are several factors to consider when assessing instability, including:
- Shallow trochlea: A shallow groove in the knee joint can contribute to patellar instability. This can be assessed through physical examination or MRI.
- High-riding patella (patella alta): This can be identified by comparing the distance between the patella and the tibial tuberosity. A high-riding patella can contribute to instability in certain ranges of motion.
- Lateralized tuberosity: A congenitally lateralized tuberosity can encourage lateral patellar movement, contributing to instability. Identifying this issue can help inform treatment priorities.
4. Addressing dynamic valgus
Dynamic valgus, or excessive inward knee movement, is often seen in individuals with patellofemoral pain. While it has been a subject of debate on social media, addressing dynamic valgus remains an essential aspect of managing patellofemoral pain.
This can be achieved by focusing on exercises that improve hip and pelvis control, as well as addressing any foot and ankle issues through the use of orthotics or other interventions.
Conclusion
Effectively managing patellofemoral pain requires a comprehensive approach that includes targeted exercises, adjuncts, and the identification of any underlying instability issues. By addressing these factors, individuals experiencing patellofemoral pain can work towards im
MD, PhD. Physical Medicine & Rehabilitation Physician from São Paulo - Brazil. Pain Fellowship in University of São Paulo.

